
Instructions for Checking Insurance Benefits
To streamline the process of billing insurance for your sessions with me, please call your own insurance carrier to inquire about the details of your benefits. We can discuss what you learn in our free Introductory Call.
I am in network with Regence BlueCross BlueShield in Oregon, Washington, Idaho and Utah, specifically these networks:
 Participating
Participating- Preferred
- Individual and Family
In Utah, I am also in-network with these Regence employer-sponsored plans: Preferred BlueOption, FocalPoint, and Preferred ValueCare networks.
I am NOT in network with Regence Legacy, Blue High Performance, MedAdvantage PPO or BlueAdvantage PPO.
In Oregon, I am also in network with First Choice Health and Providence Health Plan. My credentialing with United Healthcare is pending.

Instructions for Checking Insurance Benefits
To streamline the process of billing insurance for your sessions with me, please call your own insurance carrier to inquire about the details of your benefits. We can discuss what you learn in our free Introductory Call.
I am in network with Regence BlueCross BlueShield in Oregon, Washington, Idaho and Utah, specifically these networks:
 Participating
Participating- Preferred
- Individual and Family
In Utah, I am also in-network with these Regence employer-sponsored plans: Preferred BlueOption, FocalPoint, and Preferred ValueCare networks.
I am NOT in network with Regence Legacy, Blue High Performance, MedAdvantage PPO or BlueAdvantage PPO.
In Oregon, I am also in network with First Choice Health and Providence Health Plan. My credentialing with United Healthcare is pending.
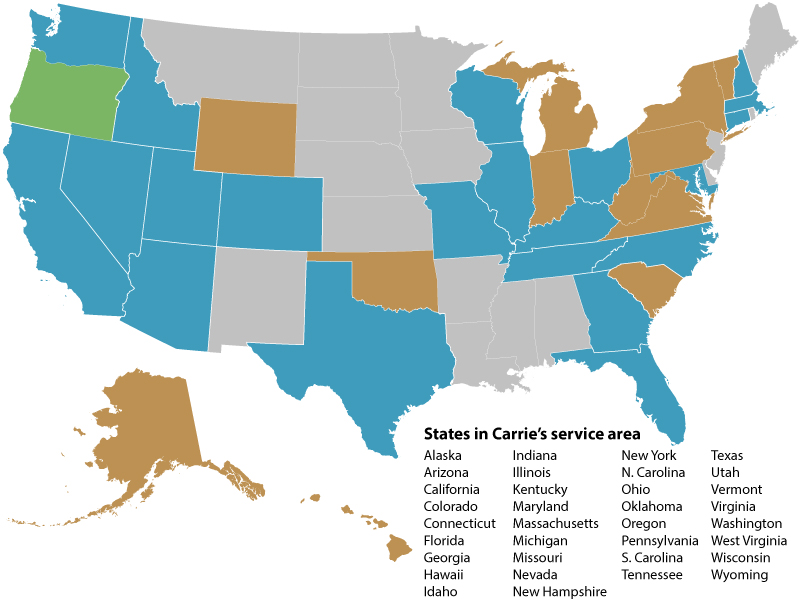
In-Network with some insurances; Carrie will provide superbill for Out-of-Network insurances
Out-of-Network, but can bill BCBS and provide superbill for other insurances
Self-Pay only
If you are in a state included in my service area and have a Blue Cross and/or Blue Shield insurance (including Premera Blue Cross in Washington state), I am out-of-network. For those, or any other insurer, you might ask about Out-of-Network benefits. If you have out-of-network benefits for nutrition counseling, I can provide you with an itemized receipt (a “superbill”) with appropriate billing codes that you can submit to your insurer to try to get partial reimbursement for your out-of-pocket costs.
You will want to have the following info handy when you call the number on the back of your insurance card:
- Provider Name: Carrie Dennett
- Provider NPI: 1326462318
- Practice Name: Nutrition By Carrie
- Practice NPI: 1336962745
Note: If you book a free introductory call, you’ll receive an electronic form that contains all the questions below, so you can simply check “yes” or “no” and type in other information while you’re on the phone with your insurance company. That allows me to have that information before our call, so we can discuss.
*Unfortunately, insurance never guarantees benefits over the phone. If a claim is denied, we will attempt to get the claim reprocessed. However, if the information that was provided to you was incorrect, then you will be responsible for the balance for the service.
What to Ask Your Insurer (for Regence, FirstChoice and Providence)
To determine your in-network benefits, call the number on the back of your insurance card and ask these questions:
- Do I have coverage for nutrition counseling? (Billing codes, also known as CPT codes, are 97802 and 97803)
- Is diagnostic code Z71.3 (dietary counseling and surveillance) covered, or is a medical diagnosis required? (If a medical diagnosis is required, I will need diagnosis documentation from your doctor.)
- Do I have a copay or coinsurance? How much is that?
- Do I have a deductible to meet before insurance pays? If so, how much of my deductible has already been met? Is the deductible waived for preventative nutrition counseling (diagnostic code Z71.3)?
- How many nutrition sessions per year does my insurance cover?
- Is there a unit limit per visit? (For example, some plans only pay for four units per visit, which would be 60 minutes.)
- Is this coverage eligible for telehealth?
- Do I need a referral or prior authorization? If so, what is the process?
- Can I have your name and a reference number? (Document this information plus the date/time of the call for future reference.)
If I Don’t Take Your Insurance
To determine if you have out-of-network benefits, you can call the number on the back of your insurance card and ask the following questions:
- Do I have out-of-network coverage for nutrition counseling? (Billing codes, also known as CPT codes, are 97802 and 97803)
- Is diagnostic code Z71.3 (dietary counseling and surveillance) covered for out-of-network claims, or is a medical diagnosis required? (If a medical diagnosis is required, I will need diagnosis documentation from your doctor.)
- Do I need a referral or prior authorization? If so, what is the process?
- Do I have a deductible to meet before insurance pays? If so, how much of my deductible has already been met? Is the deductible waived for preventative nutrition counseling (diagnostic code Z71.3)?
- How many nutrition sessions per year does my insurance cover?
- Is there a unit limit per visit? (For example, some plans only pay for four units per visit, which would be 60 minutes.)
- Is this coverage eligible for telehealth?
- How much will I be reimbursed for?
- What is the process for submitting for reimbursement? What paperwork needs to be completed and where do I send this to?
- Can I have your name and a reference number? (Document this information plus the date/time of the call for future reference.)
Out-Of-Pocket Rates
If I don’t take your insurance but you’d still like to see me, I offer out-of-pocket sessions and packages. I accept all major credit cards, in addition to HSA/FSA. If you have out-of-network nutrition coverage with your insurance, I can provide you with “superbills,” itemized receipts that you can submit to your insurance to request partial reimbursement.
I also offer a 10% discount on packages of six or more 1-on-1 sessions. Packages include access to my client portal, messaging in between sessions as needed, and custom materials tailored specifically to you and your unique goals.
Frequently Asked Questions About Payment
Will I still get charged if I miss a session?
I do have a cancellation and no-show policy that will be reviewed with you prior to starting. We understand life happens, but out of respect for other clients we do request you give me notice before canceling or rescheduling.
Can I use my HSA or FSA for nutrition counseling?
Yes!
